Bimonthly Assessment - December
This is my submission for the Bimonthly internal assessment for the month of December.
1) A 55 year old man with Recurrent Focal Seizures
Detailed patient case report here: http://ushaindurthi.
1. What is the problem representation of this patient and what could be the anatomical site of lesion ?
55 year old man presented with the right upper limb weakness and focal seizures involving right upper limb and lower limb.
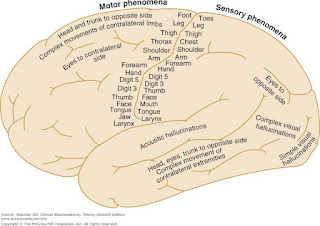
The anatomical site of lesion could be:
1.Left Frontal lobe infarct - Present as Seizures are typically brief, and can have prominent vocalization, bizarre behavior, urinary incontinence, and head and eye deviatiation
3.Left Temporal infarct - Temporal lobe seizures are characterized by behavioral arrest and impaired awareness. It is usually preceeded by aura. Aura could be sensory, emotional, cognitive, or autonomic features prior to onset of impaired awareness. Postictal confusion typically occurs.
4.Left Internal capsule infarct - Classic lacunar strokes syndrome that arises from lesions of the internal capsule are pure motor strokes, ataxic hemiparesis, and clumsy hand-dysarthria.
Sub cortical infarcts are caused by occlusion of a penetrating artery from a large cerebral artery, most commonly from the Circle of Willis. These penetrating arteries arise at sharp angles from major vessels and are thus, anatomically prone to constriction and occlusion.
So subcortical infarcts are more common than cortical infarcts.
4. What is your take on the ecg
And do you agree with the treating team on starting the patient on Enoxaparin?
ECG shows Sinus Rhythm with LAD, Left Anterior Fasciular Block with VPCS and
NSTEMI in septal leads ( seen on the day of admission -28/11/2020 and in anteroseptal leads on 30/11/2020)
5. Which AED would you prefer?If so why?Please provide studies on efficacies of each of the treatment given to this patient.
As it is focal seizure and of acute onset I would prefer carbamazepine/oxcarbazine.
To prevent secondary generalization I would add Levetiracetem.
https://www.epilepsy.com/article/2014/3/summary-antiepileptic-drugs
Question 2) 55 year old man with Recurrent hypoglycemia
1. What is the problem representation for this patient?
55 year old man, known case of hypertension and Diabetic type 2 since 10 years with metabolic syndrome
Presented with
Dyspnea on exertion since 3 days
Dry cough since 3 days
Giddiness associated with profuse sweating
2. What is the cause for his recurrent hypoglycemia? And how would you evaluate?
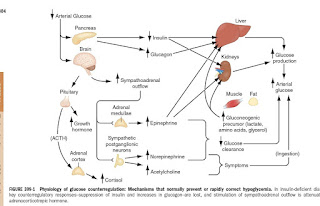
The various causes for recurring and refractory hypoglycemia can be:
3. What is the cause for his Dyspnea? What is the reason for his albumin loss?
I think the cause for his dyspnoea is renal failure.
His chest x ray also shows pleural effusion and consolidatory changes, so they may also be the reason.
https://pubmed.ncbi.nlm.nih.gov/27680887/
Albumin loss - Is clearly explained by the renal failure in this patient - with the significant spot pc ratio 3.91 and high serum creatinine 2.7mg/dl.
4. What is the pathogenesis involved in hypoglycemia ?
https://cyberleninka.org/article/n/230877
5. Do you agree with the treating team on starting the patient on antibiotics?
No, I do not agree with the treating team on starting the patient on antibiotics as he has no signs of sepsis.
A. 41 year old man with Polyarthralgia
Complete Case details here: https://
1. How would you evaluate further this patient with Polyarthralgia?
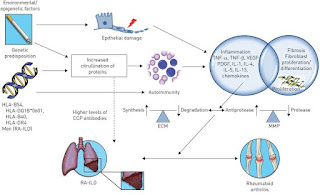
2. What is the pathogenesis involved in RA?
https://academic.oup.com/rheumatology/article/51/suppl_5/v3/1787104
3. What are the treatment regimens for a patient with RA and their efficacies
Standard recommendations suggest Methotrexate plus short-term glucocorticoids. Methotrexate should be rapidly escalated to the optimal dose (25 mg once weekly) with folate substitution to mitigate or prevent adverse events without interfering with effectiveness.
Glucocorticoids should be given at a low dose or intermediate dose for a few weeks to a maximum of 4–5 months, when methotrexate (or another conventional synthetic DMARD) should have reached full effectiveness.
Efficacy and safety of various anti-rheumatic treatments for patients with rheumatoid arthritis:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6348345/
B.
75 year old woman with post operative hepatitis following blood transfusion
Case details here: https://
1.What are your differentials for this patient and how would you evaluate?
4) 60 year woman with Uncontrolled sugars
The complete link to the case details: http://manojkumar1008.
1. What is the problem representation of this patient?
60 year old woman who is a known case of Hypertension and diabetes since 2 years with a history of AKI and septic shock 1 1/2 years back presented with the complaints of chest pain since 4 days, Abdominal pain since 3 days.
She doesn’t seem to have tachypnea, tachycardia. And she is a febrile according to the details mentioned in the elog.
Her TLC is 18,000 c/cumm on the day of admission.
Doesn’t fit into SIRS criteria.
Her CUE shows 2 plus urinary sugars loss along with uncontrolled blood sugars.
She has indirect hyperbilirubinemia with a raised ALP and reduced serum albumin.
And a slight elevation in her Serum creatinine 1.5mg/dl - ?AKI
2. What are the factors contributing to her uncontrolled blood sugars?
The measurement of her average blood sugar levels over the past 3 months (HbA1C) is 8. Her blood sugars have already not been under control owing to her irregular use of OHA'S as it was mentioned in the history.
Her blood glucose shot even further after she developed Right lung pneumonia which inturn she would be more susceptible to because of poor blood glucose control.
3. What are the chest xray findings?
The xray findings in this pt are
p/a view ,adequate exposure with opacities in right upper lobe ,with air bronchogram, with bulging fissure sign suggestive of right upper lobar consolidation.
4. What do you think is the cause for her hypoalbuminaemia? How would you approach it?
Albumin being a negative phase reactant has reduced in this acute inflammatory condition. She otherwise doesn't seem to have either renal failure or liver failure.
Or it may also be due to nutritional deficiency.
5. Comment on the treatment given along with each of their efficacies with supportive evidence.
Treatment efficacies:
Piperacillin- tazobactum.
https://pubmed.ncbi.nlm.nih.gov/9721959/
Clarithromycin:
https://journal.chestnet.org/article/S0012-3692(15)42279-2/abstract
5) 56 year old man with Decompensated liver disease.
Case report here: https://appalaaishwaryareddy.
3. What is the pathogenesis of the illness due to Hepatitis B?
4. Is it necessary to have a separate haemodialysis set up for hepatits B patients and why?
Yes.
https://www2.health.vic.gov.au/Api/downloadmedia/%7B92153955-18A8-4BBB-BFCE-413D44D5EB0C%7D
6) 58 year old man with Dementia
Case report details: http://
1. What is the problem representation of this patient?
58 year old man with Slurring of speech since 6 months
Drooling of saliva and food from the mouth since 6 months
Urinary incontinence since 6 months
Forgetfulness since 3 months
Dysphagia to both solids and liquids since 10 days
2. How would you evaluate further this patient with Dementia?
Yes
Dementia is common after stroke but we know little of the mechanisms or whether the risk varies with stroke subtype.
Stroke risk factors, amounts and regions of the brain affected, and suggested stroke mechanisms all vary with stroke subtype, and could influence the risk of cognitive impairment after stroke. For example, as cortical ischaemic strokes often affect a large area of brain, they may carry a higher risk of cognitive impairment than the smaller, less neurologically severe, lacunar strokes. Alternatively, lacunar strokes may carry a higher risk of cognitive impairment than would be expected on the basis of the lacunar infarct alone as they are part of the spectrum of cerebral small vessel disease (SVD). SVD, which affects the brain diffusely and is the commonest vascular cause of cognitive impairment, could be unmasked by a new lacunar stroke.
https://jnnp.bmj.com/content/84/8/893
4. What is the likely pathogenesis of this patient's dementia?
Post stroke dementia.
https://www.sciencedirect.com/science/article/pii/S1873959816301995
5. Are you aware of pharmacological and non pharmacological interventions to treat such a patient and what are their known efficacies based on RCT evidence?
Pharmacological:
https://pubmed.ncbi.nlm.nih.gov/20395618/
7) 22 year old man with seizures
Case report here http://geethagugloth.
1. What is the problem representation of this patient ? What is the anatomic and pathologic localization in view of the clinical and radiological findings?
22 year old man with complaints of headache since 2 months and involuntary stiffness of bilateral upper and lower limbs since 1 week along with Loss of consciousness.
Anatomical localisation - Brain
Involving both the upper limbs and lower limbs
Could be due to multiple infarcts
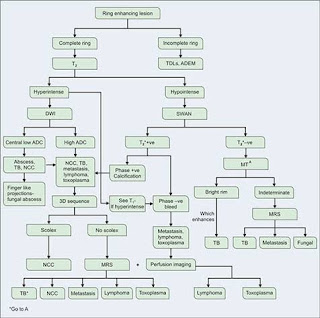
Ring enhancing lesions as he is RVD positive
Radiologically
Shows ring enhancing lesions
2. What the your differentials to his ring enhancing lesions?
3. What is "immune reconstitution inflammatory syndrome IRIS and how was this patient's treatment modified to avoid the possibility of his developing it?
A paradoxical clinical worsening of a known condition or the appearance of a new condition after initiating antiretroviral therapy in HIV-infected patients is defined as immune reconstitution inflammatory syndrome.
Despite numerous descriptions of the manifestations of IRIS, its pathogenesis remains largely speculative. Current theories concerning the pathogenesis of the syndrome involve a combination of
1. Antigenic burden
2. degree of immune restoration following
3. Host genetic susceptibility.
As his CD4 count is > 50 /mm3 consider delayed initiation of ART ideally after 8 weeks of starting ATT to reduce the chances of developing IRIS
https://cyberleninka.org/article/n/152924
8) Please mention your individual learning experiences from this month.





















Comments
Post a Comment